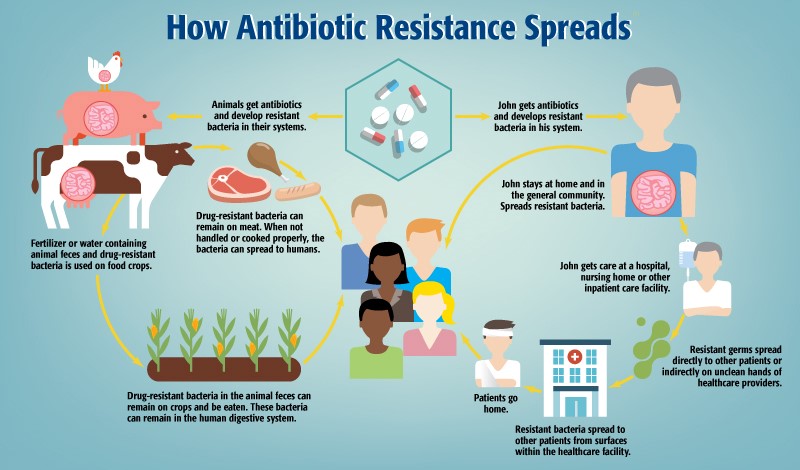
Antibiotic resistance is no longer just a human healthcare issue—it’s a shared threat across both medical and veterinary fields. As veterinarians, we stand at the front lines, where responsible antibiotic use can make a critical difference. But how exactly does antibiotic resistance develop and spread? Let’s break it down.
Step 1: Antibiotic Use in Animals
The journey begins on farms, where animals such as chickens, pigs, and cows are routinely given antibiotics. It could be from medicated feed, or disease therapy, and while this may help prevent disease and promote growth, it also creates a dangerous side effect—bacteria in the animals’ systems can become resistant to antibiotics. These drug-resistant bacteria are then carried in the animals’ bodies and waste.
Step 2: Contamination Through Food and Water
Animal waste, rich in resistant bacteria, is often used as fertilizer or finds its way into water sources. Crops grown in this environment may become contaminated. These bacteria can remain on or in the crops, making their way into the human digestive system when consumed.
Step 3: Spread Through Meat Consumption
Drug-resistant bacteria also linger on raw meat. If not properly handled or cooked, these bacteria can transfer to humans, adding another entry point for resistance to spread in the population.
Step 4: Resistance in the Community
Once in the human body, drug-resistant bacteria can settle and multiply. For example, someone like “John” may take antibiotics and unknowingly harbor resistant bacteria in his system. He then interacts with others in his household or community, unknowingly spreading the bacteria.
Step 5: Amplification in Healthcare Settings
The situation worsens if John seeks care in a hospital or nursing home. These environments often house vulnerable individuals and use intensive antibiotic treatments. Here, resistant bacteria can be spread directly from patient to patient or indirectly via the unclean hands of healthcare workers and contaminated surfaces. These healthcare facilities, intended to heal, can become hotspots for the spread of resistant germs.
Step 6: Cycle Repeats
When patients return home, they may continue to carry and transmit resistant bacteria, perpetuating the cycle. As these bacteria travel from animals to food, to people, to hospitals, and back into the community, antibiotic resistance continues to grow and evolve.
Veterinary Responsibility
To slow the spread:
- Use antibiotics only when necessary and with proper diagnostics.
- Follow strict hygiene protocols in clinics and farms.
- Educate clients on proper treatment adherence and the risks of misuse.
- Support preventive care, like vaccinations and good nutrition, to reduce infection risks.
By staying informed and vigilant, veterinarians play a crucial role in preserving antibiotic effectiveness—for both animals and people.

