Bird Sexing

Bioguard Corporation Many mammals are sexually dimorphic, which means that their sex can be identified based on their appearance. However, it is not the case for most birds. Many birds are sexually monomorphic although males and females may differ markedly in size, color, and appearance in some birds, such as peacocks (Fig. 1). Knowledge of […]
Polyomavirus in Birds

Long Pham Avian polyomavirus in birds poses a significant concern for caged birds, leading to substantial economic losses for pet retailers and bird enthusiasts. Initially identified in budgerigars during the early 1980s in Ontario, Canada and in the southern regions of the United States, it was initially termed Budgerigar Fledgling Disease Virus. This nonenveloped DNA […]
Severe Fever with Thrombocytopenia Syndrome
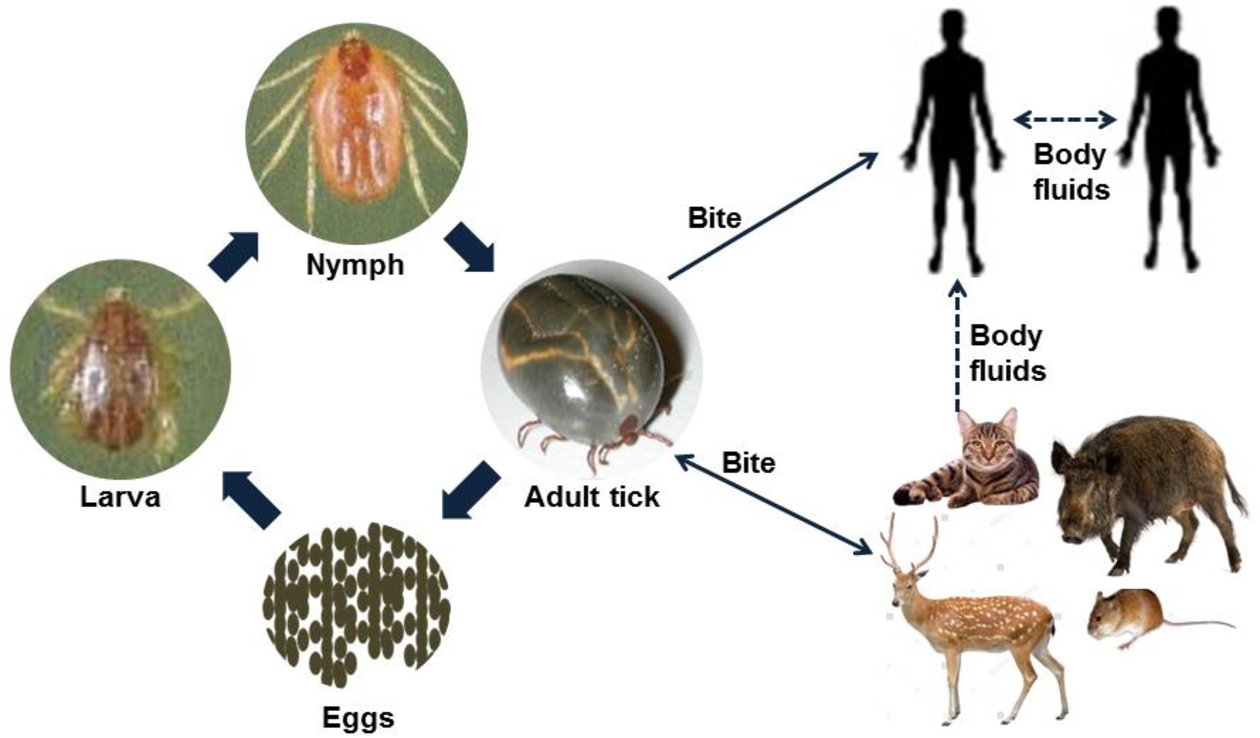
Bioguard Corporation Severe Fever with Thrombocytopenia Syndrome (SFTS) is an emerging infectious disease that was first reported in China in 2011. It is caused by the Severe Fever with Thrombocytopenia Syndrome virus (SFTSV) and is transmitted to humans and animals through the bite of an infected tick. The main clinical symptoms of SFTS include fever, […]
Cryptosporidiosis

Bioguard Corporation Cryptosporidiosis is an illness you get from the parasite Cryptosporidium. It causes watery diarrhea and other gastrointestinal (gut) symptoms. In addition to stomach infection, this parasite can infect the respiratory system causing a cough and/or problems breathing. The family Cryptosporididae belongs to the phylum Apicomplexa characterized by an anterior (or apical) polar complex […]
Ferret Coronavirus

Bioguard Corporation The coronavirus of ferrets was first described in 1993. This ferret enteric coronavirus (FRECV) caused an enteric disease called epizootic catarrhal enteritis (ECE) or green slime disease. Later, a ferret systemic coronavirus (FRSCV)-associated disease, resembling the dry form of feline infectious peritonitis (FIP), was identified. ECE is characterized by high morbidity (nearly 100%) […]
Infectious Myxomatosis of Rabbits

Bioguard Corporation Myxomatosis is primarily a disease of rabbits caused by infection with the myxoma virus. It mainly occurs in domestic and wild rabbits. The virus is harmless to humans. Myxomatosis can result in lumps developing around the ears and face. These lumps are named myxomas and the disease virus was named after this lesion. […]
Diagnosis of Feline Respiratory Mycoplasma Infection

Bioguard Corporation In cats, ’mucosal’ mycoplasma infections typically cause ocular and respiratory disease, and less frequently neurological or joint disease. These Mycoplasma species are distinct to the haemotropic mycoplasmas that target red blood cells, causing hemolytic anemia in cats. Mycoplasma felis is typically associated with Upper Respiratory Tract Disease (URTD) in cats. Transmission M. felis […]
Tritrichomonas Infection in Cat
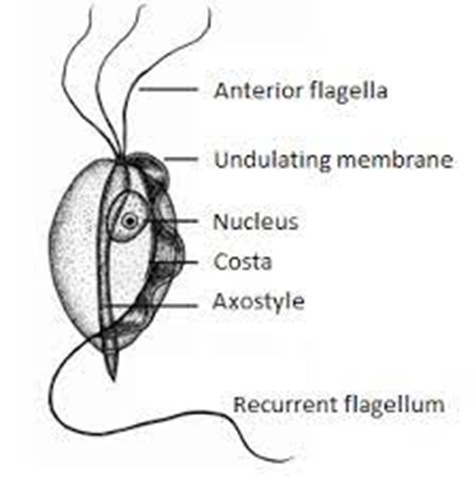
Bioguard Corporation Tritrichomonas foetus is a significant cause of large bowel diarrhea and persistent colitis in cats. These pear-shaped organisms have three anterior flagella and one posterior flagellum. They have a distinctive undulating membrane, which gives them a similar appearance to Giardia. However, they do not form cysts and are transmitted directly from one host […]
Encephalitozoon cuniculi in Rabbits

Bioguard Corporation Encephalitozoon cuniculi is a microsporidial, unicellular, spore-forming, obligate intracellular parasite. It can invade the host’s central nervous system, kidneys, crystals, etc. E. cuniculi affects rabbits by causing damage to the brain, nervous system, kidneys, and other important organs. E. cuniculi pose a zoonotic risk to immune-compromised humans. In addition, it can infect various […]
Psittacosis in Birds

Bioguard Corporation Psittacosis (parrot fever), also known as ornithosis, is a bacterial zoonotic disease caused by the bacterium Chlamydia psittaci. It is usually spread by exposure to infected birds at home, pet stores, pigeon stalls and other locations where birds are kept or displayed. The disease was first reported in Switzerland in 1879, and then […]