Protecting Dogs from the Threat of Leptospirosis

Leptospirosis is a zoonotic bacterial disease caused by pathogenic spirochetes of the genus Leptospira. It affects a wide range of mammals, including domestic animals, wildlife, and humans. Leptospira are aerobic, gram-negative spirochetes characterized by their corkscrew-like motility. These bacteria are slow-growing and can survive for weeks to months in warm, moist environments such as […]
What is the Danger of AMR in animals?

Antimicrobial resistance (AMR) occurs when microorganisms—such as bacteria, viruses, fungi, and parasites—adapt to withstand medications designed to eliminate them or inhibit their growth. This phenomenon reduces the effectiveness of treatments, making infections more difficult to control and increasing the risk of disease transmission, severe illness, and mortality. For veterinarians, understanding AMR is essential due to […]
WHAT ARE THE FACTORS THAT AFFECT “ANTIBIOTIC RANK”?

Factors Influencing the Ranking of Veterinary Antibiotics Resistance Potential One of the most critical factors in ranking veterinary antibiotics is their potential to promote antibiotic resistance. Drugs like fluoroquinolones and third-generation cephalosporins are closely monitored because of the risk that resistant strains can transfer from animals to humans through food consumption or direct contact. Spectrum […]
Feline Herpesvirus 1 (FHV-1) Infection

Bioguard Corporation Feline herpesvirus-1 (FHV-1) is a common viral infection in cats that primarily affects the upper respiratory system. It is a major cause of feline viral rhinotracheitis (FVR), which presents symptoms like sneezing, nasal discharge, and conjunctivitis (eye inflammation). FHV-1 is highly contagious among cats and is spread through direct contact with infected saliva, […]
WHAT DOES “ANTIBIOTIC RANK” MEANS?

The use of antibiotics is critical to maintaining both human and animal health, ensuring food safety, and preventing the spread of zoonotic diseases. However, concerns about antibiotic resistance have prompted the need to rank veterinary antibiotics based on their importance, usage, and associated risks. This ranking or categorization serves as a tool to support veterinarians […]
Understanding Antibiotic Classifications: A Comprehensive Guide
Antibiotics are essential tools in modern medicine, used to combat bacterial infections that could otherwise lead to severe health issues or even death. To use these powerful drugs effectively, it’s crucial to understand the different classifications of antibiotics, which are based on their chemical structure, mechanism of action, and spectrum of activity. This article explores […]
Fowl Pox

Bioguard Corporation Fowl pox is a slow-spreading viral disease affecting chickens, turkeys, and various other birds. It is characterized by proliferative skin lesions that develop into thick scabs (cutaneous form) and lesions in the upper respiratory and digestive tracts (diphtheritic form). A presumptive diagnosis can be made in the field based on distinctive skin lesions, […]
Factor VII Deficiency in Dogs

Bioguard Corporation Canine Factor VII (FVII) deficiency is an autosomal recessive genetic disorder that leads to a mild to moderate blood clotting problem in affected dogs. Puppies with the condition may exhibit symptoms such as nosebleeds (epistaxis) and gum bleeding, while adult dogs are more prone to bruising and skin issues like dermatitis. Though bleeding […]
Pyruvate Kinase Deficiency in Dogs

Bioguard Corporation Pyruvate kinase deficiency (PKD) is a hereditary genetic disorder that impairs the ability of red blood cells to metabolize properly. This defect leads to the destruction of red blood cells, resulting in severe hemolytic anemia. Affected animals can die from complications such as severe anemia and liver failure. The condition typically manifests between […]
Juvenile Hereditary Cataracts in Dogs
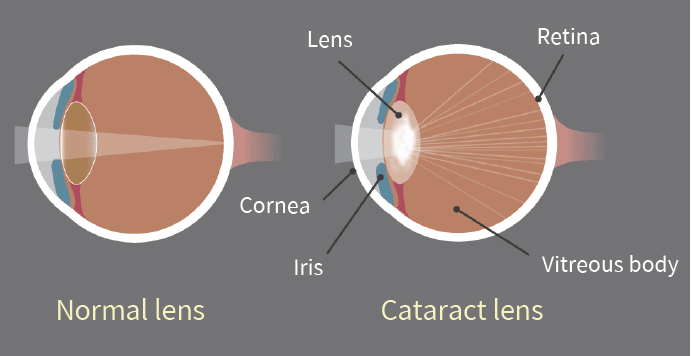
Bioguard Corporation Canine juvenile cataract (JHC) is a hereditary form of cataract characterized by cloudiness and degeneration of the lens in the eye. This condition prevents light and images from passing through the lens to the retina, impairing the dog’s vision and eventually leading to blindness. Affected dogs may exhibit symptoms such as bumping into […]