Infectious Myxomatosis of Rabbits
Bioguard Corporation Myxomatosis is primarily a disease of rabbits caused by infection with the myxoma virus. It mainly occurs in domestic and wild rabbits. The virus is harmless to humans. Myxomatosis can result in lumps developing around the ears and face. These lumps are named myxomas and the disease virus was named after this lesion. It was first discovered in South America, California and Mexico in 1896. Sick animals will die within a few days to two weeks after infection, and the fatality rate is close to 100%. Currently, there is no effective treatment. Pathogen Myxoma virus is the type species of the Leporipoxviruses, a genus of Chordopoxvirinae, double stranded DNA viruses, whose members infect leporids and squirrels, inducing cutaneous fibromas from which virus is mechanically transmitted by biting arthropods. Pathogenesis studies confirm that the virus initially replicates in dermal cells at the inoculation site, likely dendritic cells. From there, the virus spreads to local macrophages and epidermal cells, and to the draining lymph node. Virus replication in the latter results in lymphoid depletion, with extensive loss of cortical and paracortical lymphocytes. From the lymph node the virus spreads via blood leukocytes to distal tissues including the spleen and other lymphoid tissues, testis, lungs, and skin. Transmission and Clinical Signs Currently, myxoma virus is enzootic to the Americas, Europe, Australia and other regions. The principal mode of transmission of the virus is mechanical transport of virus on mouth parts by arthropod vectors such as ticks, mosquitoes, and fleas through bites. It can also transmit the virus to other rabbits via direct contact. The general incubation period is 3-7 days, up to 14 days. The first sign of disease is conjunctivitis that rapidly becomes more severe and is accompanied by a milky discharge from the eye. The rabbit has no energy and no appetite, with a fever that may reach 42°C. In severe outbreaks, some rabbits die within 48 hours after signs appear. Those that survive become progressively weaker and develop a rough coat. The eyelids, nose, lips, and ears become puffy, which gives a swollen appearance to the head. The ears may droop. In females, the vulva becomes inflamed and swollen with fluid; in males, the scrotum swells. Other signs include discharge of pus from the nose, difficulty breathing, and coma. Death usually occurs within 1 to 2 weeks after signs appear, and the fatality rate is close to 100%. Diagnosis Gross lesions: The most prominent gross lesions in in rabbits with myxomatosis are the skin tumors and the pronounced cutaneous and subcutaneous edema, particularly in the area of the face and around body orifices. Hemorrhages of the skin, heart, and subserosa of the gastrointestinal tract may be observed. Microscopic lesions: Lesions in the skin involve epithelial cells, fibroblasts, and endothelial cells and range from proliferative to degenerative, depending on the strain of virus. The skin tumors result from proliferation of undifferentiated mesenchymal cells, which become large stellate (myxoma) cells surrounded by a homogeneous matrix of mucinous material interspersed with capillaries and inflammatory cells Lab tests include serology and molecular diagnosis. Serology: immunofluorescent assay (IFA), ELISA, complement fixation test (CFT) Molecular diagnosis: PCR Treatment and Vaccination Unfortunately, there is no specific treatment for myxomatosis. Vet can only offer supportive care, including fluids, antibiotics to prevent secondary infections, and pain medication. The myxomatosis vaccine is available in some countries. Reference Bertagnoli S, Marchandeau S. Myxomatosis. Rev Sci Tech. 2015 Aug;34(2):549-56. Espinosa J, Ferreras MC, Benavides J, et al. Causes of Mortality and Disease in Rabbits and Hares: A Retrospective Study. Animals (Basel). 2020 Jan 17;10(1):158.
Encephalitozoon cuniculi in Rabbits

Bioguard Corporation Encephalitozoon cuniculi is a microsporidial, unicellular, spore-forming, obligate intracellular parasite. It can invade the host’s central nervous system, kidneys, crystals, etc. E. cuniculi affects rabbits by causing damage to the brain, nervous system, kidneys, and other important organs. E. cuniculi pose a zoonotic risk to immune-compromised humans. In addition, it can infect various mammals, such as rabbits, rats, mice, horses, foxes, cats, dogs, muskrats, leopards, and baboons. Transmission and Life Cycle E. cuniculi has a direct life cycle with both horizontal and vertical (transplacental) transmission. In rabbits, the common routes of natural horizontal infection are via the ingestion of contaminated food or water or, less commonly, via inhalation of spores. After ingestion, the spores invade enterocytes and then spread through bloodstream or the lymphatic system. Then, it is carried into the blood circulation to target organs (kidney, central nervous system, eye, liver, and heart) where it causes inflammation. Antibody can be detected 2-3 weeks after infection, and IgM are usually detectable up to 18 weeks post-exposure. Spores are passed in the urine of rabbits, beginning around 35 days after infection, and continue to be excreted for 2 to 3 months. Serological surveys show high seroprevalence rates (23-75%) of E. cuniculi in rabbits. The seroprevalence rate of E. cuniculi is about 63.2-67.8% in Taiwan. However, most are asymptomatic and few are found to be affected by disease. Clinical signs When E. cuniculi infect the rabbits, the common clinical signs include head tilt (vestibular disease), hind limb paresis (weakness of the hind limbs), urinary incontinence, renal failure, cloudy eyes (anterior uveitis), cloudy lenses of the eyes (cataracts), or even blindness. Diagnosis Clinical diagnosis of encephalitozoonosis can be challenging because of the following reasons. 1. Serologic evidence is strong evidence of infection but not indicative of clinical signs. 2. Seroconversion does not result in a protective response for the patient. 3. Histologic severity and distribution of lesions are not directly correlated with the severity of clinical signs. 4. Most infected rabbits are asymptomatic or carriers. Diagnostic methods of encephalitozoonosis include histopathology, serology, and molecular diagnosis. • Histopathology- histological examination combined with special staining, or concentrated urine for cytological microsporidia detection • Serology- indirect immune fluorescence antibody test, direct agglutination test, ELISA, western blot • Molecular diagnosis- PCR Treatment and Prevention No uniformly effective treatment has been established. Fenbendazole, Albendazole, and Oxibendazole may be effective in vivo. The treatment of choice generally is fenbendazole, because it has been shown to both prevent and treat E cuniculi infections. To reduce the inflammatory reaction, steroids or NSAIDS may be applied. The use of systemic steroid therapy, although controversial, has been advocated to reduce severe CNS inflammation. The risk with this treatment is that corticosteroids might suppress the immune system to the point that E cuniculi or other infectious organisms may create additional problems. Cases involving the ocular form need to be referred to a veterinary ophthalmologist if surgery is recommended. Prevention of the disease from spreading includes thoroughly cleaning the rabbit’s environment, applying a diluted solution of bleach (1:32) for disinfection, and providing clean water and food to rabbits.
Rabbit Hemorrhagic Disease

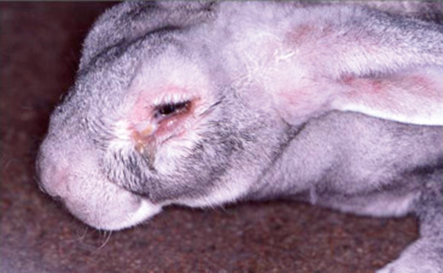
Long Pham Introduction Rabbit hemorrhagic disease (RHD) is a highly contagious and lethal viral disease caused by a virus from the Caliciviridae family. This disease seems to only affect European rabbits (Oryctolagus cuniculus),both domesticated and wild rabbits. However, a newer strain of the virus, RHDV2, can affect rabbits with previous immunity to RHD and also hares (Lepus spp.). The first outbreak of rabbit hemorrhagic disease was noted in China from a shipment of Angora rabbits from Germany in 1984 (1). The devastating nature of this disease can be seen as about 140 million domestic rabbits were killed in China during this outbreak in just less than a year (1). The next country to have an RHD outbreak was Korea due to importing rabbit fur from China (2). In 1986, the disease arrived in Italy and then spread to the rest of Europe (3). In 1988, the first outbreak in the Americas was reported in Mexico from imported rabbit products coming from China (4). However, Mexico was able to control RHD and had its last outbreak in 1992 (4). While RHD has been seen as a devastating disease that causes ecological and economical impacts, for New Zealand and Australia, RHD was considered as a method of pest control for the wild rabbits (5). Rabbit hemorrhagic disease virus was released in Wardang Island in South Australia, but in 1995, RHDV escaped and reach Australia (6). At the moment, RHD generally occurs in areas where European rabbits are found in the wild, with deadly outbreaks that can occur on almost all continents. Clinical signs Rabbit hemorrhagic disease virus has an incubation period of around 1-3 days. The virus can affect many internal organs (mainly targets the spleen, liver, and lungs), causing internal bleeding in infected rabbits. This disease can be present in 3 different forms: peracute, acute, subacute. Peracute form: Infected rabbit dies suddenly without showing any signs. Can be seen functioning normally before suddenly dying. Acute form: Rabbits can have a lack of motivation to move, ataxia, convulsions, subconjunctival hemorrhage, respiratory issues, and nosebleeds (Figure 1). For these infected rabbits, death can occur within 72 hours. Subacute form: These rabbits can have the same symptoms, but in a milder form. In this form, liver damage can occur, causing jaundice, with death that can occur weeks later. In general, most rabbits survive and develop some immunity to the virus. In general, rabbits that have clinical symptoms will die from the disease, while rabbits with the subacute form may survive. Rabbits that recover from the subacute form may have extensive liver damage, resulting in chronic liver diseases. Diagnosis Rabbit hemorrhagic disease can be confirmed through a post-mortem examination for the presence of an enlarged and pale liver. Molecular testing of live samples with PCR or ELISA can also confirm diagnosis. However, some tests may not be able to distinguish between RHDV and RHDV2. Figure 1: Rabbits with RHD often die suddenly and have bleeding from the nose due to internal bleeding. (Photo Credit: Dr. J.P. Teifke from theFederal Research Institute for Animal Health in Riems, Germany) Treatment and Disease Control Rabbit hemorrhagic disease have several possible routes of transmission: nasal, oral, conjunctival, and through other places because hematophagous insects have been seen to be quite effective in spreading diseases (7). Rabbit hemorrhagic disease virus may be shed through the rabbit’s excretions and secretions, making direct contact with or contact with contaminated environment the likely method of transmission. The remains of infected rabbits may also be a source of infections and spreading of the virus because it is very resilient and has been seen to still be viable even after three months (8). Flies and birds can also be effective carriers of the virus because they can travel great distances with the resilient virus and contaminate the rabbit’s food source and habitat. Carnivores and scavengers are other possible carriers because the virus from consumed infected rabbits can transported and spread through the feces. Currently, there is no cure for rabbit hemorrhagic disease. Supportive care may help, but it’s best to have preventive care with vaccinations. Hyperimmune antiserum can be effective if the rabbit has not showed clinical signs, but will be ineffective after the signs appear. For domestic rabbits, vaccinations is an effective preventative measure. However, for wild rabbits, the sheer number of rabbits would make vaccinations economically unfeasible at the moment. To help prevent outbreaks, countries can place bans or restrictions on importing rabbit products, such as meats or furs, from other countries where rabbit hemorrhagic disease is endemic. Other preventative methods are culling, monitoring, following strict quarantining rules, and thoroughly disinfecting contaminated areas before bringing rabbits there again. Disinfection of the rabbit hemorrhagic disease virus can be done with a 4-10% solution of sodium hydroxide or 1-2% formalin solution. A 1:10 dilution of household bleach can also be used for disinfecting infected surfaces. However, since the virus is nonenveloped, an alcohol-based disinfection is not effective. Reference 1. Liu, S. J., H. P. Xue, B. Q. Pu, and N. H. Qian. 1984. A new viral disease in rabbits. Animal Husbandry and Veterinary Medicine (Xumu yu Shouyi) 16:253–255. 2. Park, N.Y., C. Y. Chong, J. H. Kim, S. M. Cho, Y. H. Cha, B. T. Jung, D. S. Kim, J. B. Yoon, J. Y. Park, and S. H. Wee, 1987. An outbreak of viral haemorrhagic pneumonia (tentative name) of rabbits in Korea. Journal of the Korean Veterinary Medical Association: 23: 603-610. 3. Cancellotti, F. M., and M. Renzi. 1991. Epidemiology and current situation of viral haemorrhagic disease of rabbits and the European brown hare syndrome. Revue Scientifique et Technique de l’OIE 10:409–422. 4. Gregg, D. A., C. House, and M. Berninger. 1991. Viral haemorrhagic disease of rabbits in Mexico: Epidemiology and viral characterization. Revue Scientifique et Technique de l’OIE 10:435–451. 5. Cooke, B. D. 2002. Rabbit haemorrhagic disease: Field Epidemiology and the management of wild rabbit populations. Revue Scientifique et Technique de l’OIE 21:347–358. 6. Cooke, B. D., and F. Fenner. 2002. Rabbit